This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment.
1601006162
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment.
SHORT CASE
A 53yrs old male patient farmer by occupation hailing from Nakrekal came with the chief complaints of Shortness of breath since 4 months and pedal edema of left leg since 4 months
History of present illness
Patient was asymptomatic 4 months back then he had a minor trauma to the left leg after which he developed swelling and pain around the foot which gradually increased up to the leg for which he visited a local RMP there incision and drainage of swelling was done and he was admitted for 15 days. But the swelling of the leg was not completely treated
After few days from this incident he developed distension of abdomen, shortness of breath which is present at rest (grade 4) and he also developed jaundice for which he visited a hospital in Hyderabad there he was diagnosed with liver disease. He was treated for one month in the hospital and all his symptoms were relieved
After 1 month after relief from symptoms he drank alcohol after which he developed shortness of breath and distension of abdomen for which he was treated again and medication were given
At present he has shortness of breath of grade 3 and swelling of left leg
No history of chest pain
No history of palpitations
No history of orthopnea and PND
No history of cough
Past history
He was diagnosed with diabetes mellitus 3months back and is under medication
Not a known case of hypertension, bronchial asthma, tuberculosis
Family history
No history of similar complaints in family
No history of diabetes mellitus, hypertension, bronchial asthma
Personal history
Diet: mixed
Appetite: normal
Sleep: adequate
Bowel and bladder movements: regular
He is an alcoholic since 30years.
General examination
Patient is conscious coherent and cooperative moderately built and moderately nourishment
Icterus is present
Pallor is absent
Clubbing :absent
Cyanosis: absent
Koilonychia: absent
Edema: present in left leg
Vitals
Temperature: Afebrile
Pulse: 80bpm regular, normal in volume and character. There is no radio-radial or radio-femoral delay.
Respiratory rate: 20cpm
BP: 110/70mmHg in left arm in sitting position
On inspection of left leg
Left leg has swelling with discharge
Abdomen examination
Inspection:
Abdomen is distended
Umbilicus is central
All quadrants are moving with respiration
No sinus and engorged veins
Palpation
No local rise of temperatures and tenderness
Hepatomegaly is present
Splenomegaly is present
Percussion
Fluid thrill and shifting dullness is absent
Auscultation
Bowel sounds are heard
CVS Examination
Inspection
Chest wall appear symmetricalTrachea appears to be in midline
Palpation
Trachea midline
No carotid thrill
Apex beat: 5th intercostal space in midclavicular line
No epigastric pulsations
No tenderness
Auscultation
S1 heard
S2 heard
Respiratory System
Inspection
Trachea appears to be central
Elliptical and bilaterally symmetrical chest
Palpation
Trachea is central in position
Both sides move equally with respiration
No tenderness
Percussion
Resonant note heard in all areas
Auscultation
Normal vesicular breath sounds heard
Bilateral air entry is present
Investigations
Complete Blood Picture
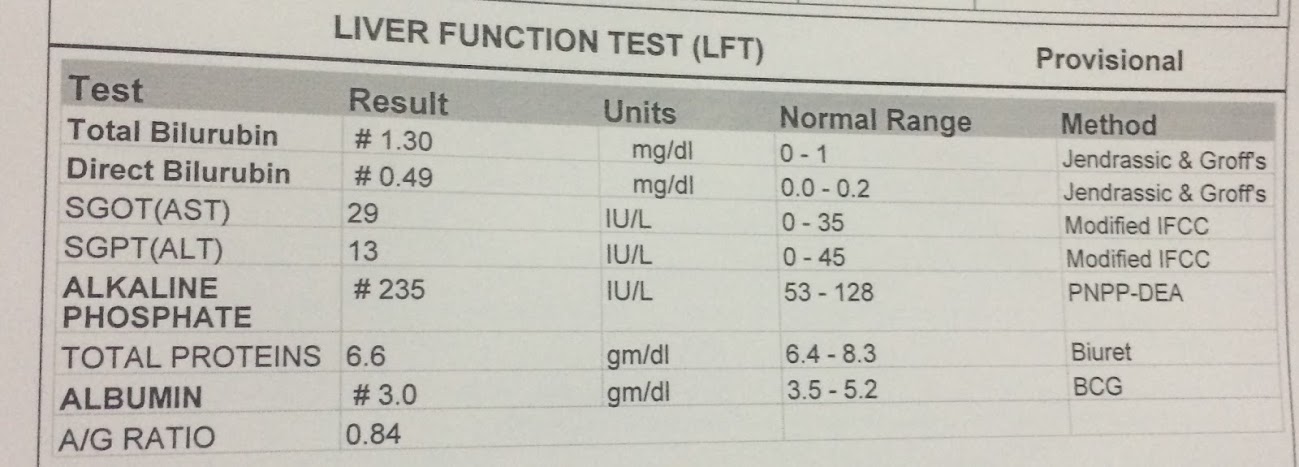
Liver function test
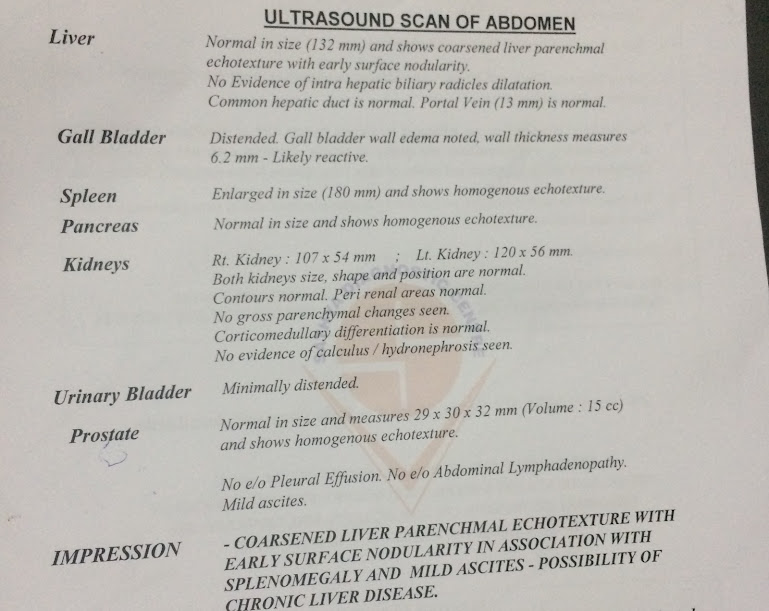
Ultrasound Abdomen
Blood Sugars
Provisional diagnosis
Since patient has shortness of breath, jaundice, abdominal distension and hepatosplenomegaly my anatomical diagnosis is liver
After performing investigations diagnosis is confirmed as chronic liver disease with portal hypertension
Left lower limb cellulitis.





Comments
Post a Comment