PARAPARESIS
"I've been given this case
https://srianugna.blogspot.com/2020/05/hello-everyone.htmll
https://youtu.be/3VVH7w3rWSM
to solve in an attempt to understand the topic of "paraparesis."
This may develop my competency in
a) reading and comprehending clinical data related to "paraparesis" including history, clinical findings, investigations
b) come up with a diagnosis such as:
1) Anatomical location of the root cause
2) Physiological functional disability
3) Biochemical abnormalities that could be a root cause at a molecular level
4) Pathology that could reflect the root cause at a cellular level
c) a treatment plan for each of these patients of paraparesis that can have a pharmacological and non pharmacological component.
d) learning the scientific basis of diagnostic and therapeutic approach in terms of past collective experiences and experiments (aka evidence based medicine).
Following is my analysis of patient's problem.
Patient is 18 year old came with the complaint of bilateral lower limb weakness which is chronic and insidious and progressive in nature.With this complaint of weakness what comes to my mind is invovement of nervous system.
Patient did not have any of the above conditions, so I RULE OUT LESION OF BASAL GANGLIA.
(This image is taken from http://www.ajnr.org/content/37/6/1005)
If there is lesion this area, patient can present with following signs and symptoms:
As this is LMN lesion next step is to know at which site of lower motor neuron pathology is present.
signs and symptoms
History related to present case
https://srianugna.blogspot.com/2020/05/hello-everyone.htmll
https://youtu.be/3VVH7w3rWSM
to solve in an attempt to understand the topic of "paraparesis."
This may develop my competency in
a) reading and comprehending clinical data related to "paraparesis" including history, clinical findings, investigations
b) come up with a diagnosis such as:
1) Anatomical location of the root cause
2) Physiological functional disability
3) Biochemical abnormalities that could be a root cause at a molecular level
4) Pathology that could reflect the root cause at a cellular level
c) a treatment plan for each of these patients of paraparesis that can have a pharmacological and non pharmacological component.
d) learning the scientific basis of diagnostic and therapeutic approach in terms of past collective experiences and experiments (aka evidence based medicine).
Following is my analysis of patient's problem.
Patient is 18 year old came with the complaint of bilateral lower limb weakness which is chronic and insidious and progressive in nature.With this complaint of weakness what comes to my mind is invovement of nervous system.
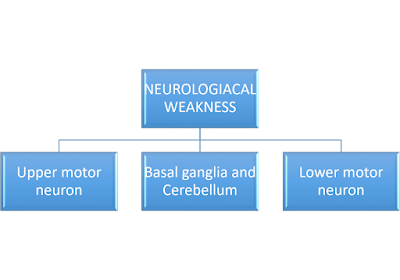
Neurological cause of weakness can be related to following anatomical structures,
Any lesion in the motor system can lead to :
- plegia
- paresis - In this patient it is paraplegia(bilateral lower limb weakness)
- involuntary movements
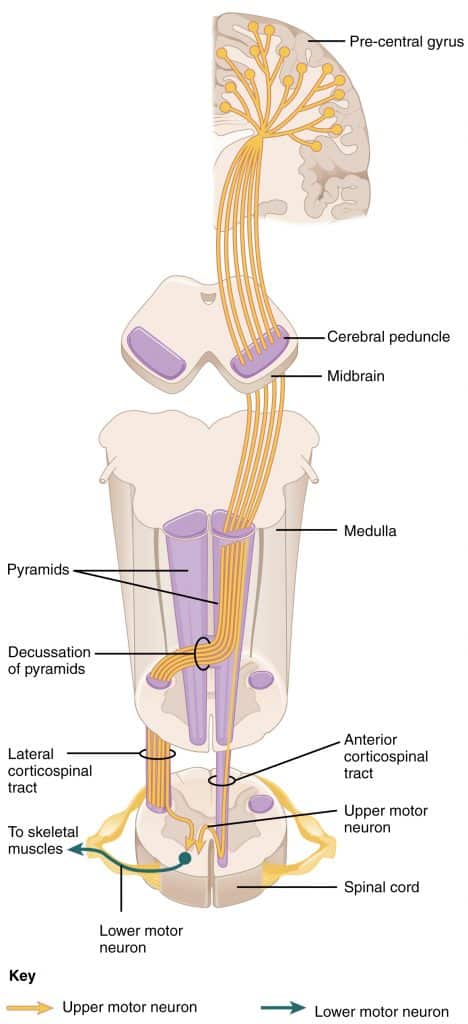
UPPER MOTOR NEURON
A neuron that extends from cerebral cortex(motor) to brainstem or spinal cord is known as upper motor neuron.
If there is lesion in this area, patient can present with following signs and symptoms:
- mostly distal muscle involvement
- apraxia
- flexor weakness in lower limb
- no muscle atrophy
- hypertonia
- spasticity(clasp knife spasticity)
- deep tendon reflexes are exaggerated
- babinki is present
- clonus:sustained
- abdominal reflexes are absent
History related to present case
- history of difficulty in performing squatting
- history of wearing and holding of chappal
- no history of difficulty in buttoning and unbuttoning shirt -suggestive of no distal muscle involvement in upper limb
- no history of difficulty in combing hair-suggestive of no proximal muscle involvement on upper limbs
- muscle atrophy is present-not suggestive of UMN lesion
- hypotonia is present-not suggestive of UMN lesion
- reflexes are absent-not suggestive of UMN lesion
BASAL GANGLIA
Basal ganglia is mainly involved voluntary control of movements.Lesion is the basal ganglia can present as following:- Athetosis
- Chorea
- Ballismus
- Dystonia
- Resting tremors
- Bradykinesia
- Rigidity
Patient did not have any of the above conditions, so I RULE OUT LESION OF BASAL GANGLIA.
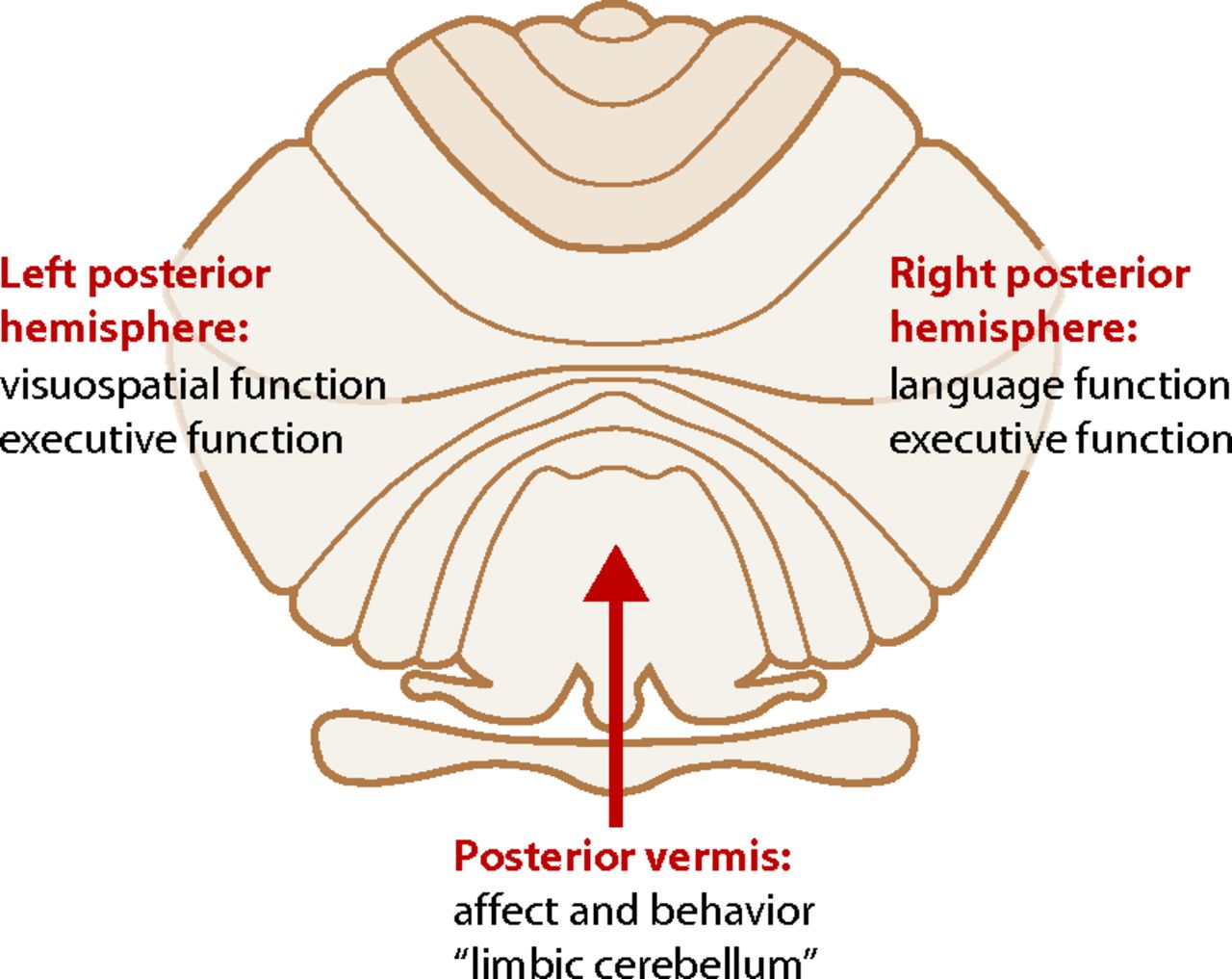
CEREBELLUM
Cerebellum is mainly involved in motor learning,sense of body position,fine movement coordination,balance and equilibrium.
Lesion in cerebellum can present with following signs:
- Dysmetria
- Dysdiadokinasia
- Gait abnormalities
- Hypotonia
- Dysarthria
- Nystagmus
- Intension tremors
- Pendular knee jerk
History related to present case
- ataxic gait is not present (For more informaation about gait- https://stanfordmedicine25.stanford.edu/the25/gait.html)
- no history of any other above mentioned signs
(This image is taken from http://www.ajnr.org/content/37/6/1005)
LOWER MOTOR NEURON
A neuron that extends from spinal cord or brainstem to muscle is know as lower motor neuron.- mostly proximal muscle are involved
- atrophy of mucles
- flaccidity
- hypotonia
- deep tendon reflexes are reduced or absent
- babinski is negative
- fasiculations and fibrillations are present
- history of weakness in proximal region followed by distal region (lower limb) is present
- atrophy is present
- deep tendon reflexes are absent(areflexia)
As this is LMN lesion next step is to know at which site of lower motor neuron pathology is present.
signs and symptoms
History related to present case
- history of symmetrical weakness of lower limbs
- history of proximal muscle weakness followed by distal muscle weakness
- no history of loss of sensation( no H/O numbness,tingling,pin and needles sensation,burning pain,tight band like pressure and insensitivity to cold)
- areflexia is present
- Myopathy
- Demyelinating peripheral neuropathy
Demyelinating peripheral neuropathy
It is the involvement of demyelinated neurons.In the present case as it is chronic paraplegia it could be CIPD.
Signs and symptoms
- Both proximal and distal weakness
- Areflexia
- No atrophy
- Motor system is predominent than sensory
- CSF analysis-increase in protiens
- EMG and NCS-latency and decreased conduction velocity
As EMG is normal there is no invovement of peripheral nerves.So I RULE OUT CIPD.
MYOPATHY
History related to present case
- history of persistent bilateral weakness of proximal lower limb followed by distal
- buckling gait
- no history of any drug intake
- history of pedal edema is present
- cardiomyopathy is present
- Polymyositis
- Hypothyriodism
- Becker muscular dystrophy
Investigations:
I would like to order following investigations:
- Thyroid profile
- muscle biopsy to find any inflammatory cause
- Chest X -ray
- CPK
- EMG
- genetic testing for becker muscular dystrophy
- Muscle biopsy
Muscle biopsy rules out polymyopathy.
BECKER MUSCULAR DYSTROPHY
It is a X-linked recessive inherited dystrophy characterized by weakness and wasting of skeletal and cardiac muscles.It is caused by DMD gene mutation.It has variable disease onset.
Signs and symptoms
- muscle wasting
- cardiomyopathy
- arrythmias
- scoliosis
- features of myopathy
- CK-MB
- EMG
- Muscle biopsy
- Chest x-ray
- genetic testing
Edits:
As NCS are normal,I rule out CIPD.
Reference:
The above mentioned information, charts and tables are written after watching Marrow and reading, and understanding from Harrison's principles of internal medicine.
Michael J. Aminoff. Neurological Causes of Weakness and Paralysis and Numbness, tingling, and sensory loss.In:D.L Kasper, S.L. Hauser,D.L.Longo, J.L.Jameson, J.Loscalzo, A.S.Fausi. Harrison's principles of internal medicine.20th ed. New York: McGraw-Hill;2018.Pg 135-143
Daniel H. Lowenstein; Joseph B. Martin; Stephen L. Hauser. Approach to patient with neurological disease. In:D.L Kasper, S.L. Hauser,D.L.Longo, J.L.Jameson, J.Loscalzo, A.S.Fausi. Harrison's principles of internal medicine.20th ed. New York: McGraw-Hill;2018.Pg 3025-3030
Anthony A. Amato; Richard J. Barohn. Peripheral neuropathy. In:D.L Kasper, S.L. Hauser,D.L.Longo, J.L.Jameson, J.Loscalzo, A.S.Fausi. Harrison's principles of internal medicine.20th ed. New York: McGraw-Hill;2018.Pg 3204-3225.
.






👍"As EMG is normal there is no invovement of peripheral nerves.So I RULE OUT CIPD."
ReplyDeleteThis will be NCV not EMG
I will change it sir
Delete